2023 Pilot Awardee Spotlight

Max M Aung, PhD, MPH
Project Title: Air pollution, community-level social and neighborhood factors, and depression and anxiety in
children of US born and immigrant parents (Co-I: Carlos Cardenas-Iniguez)
I earned my PhD in Environmental Health Sciences at the University of Michigan School of Public Health. I’m currently an Assistant Professor in the Division of Environmental Health here at USC. Some academic things about me are that I care deeply about strengthening opportunities for historically marginalized trainees in health science fields and pursuing research that can be used to advance environmental justice.
I am motivated to pursue this project to advance understanding of the joint environmental and social contributors of neurobehavioral health, particularly among immigrants in the US. This project is a great opportunity to investigate air pollution and social factors in relation to neurobehavioral health in children with immigrant parents and those with US born parents. Through this research, we can better inform risk assessment and interventions in historically marginalized communities.
I am really thankful for the opportunity to pursue this project, and excited to learn about all of the other funded pilot projects!

Carlos Cardenas-Iniguez, PhD, MA
Project Title: Air pollution, community-level social and neighborhood factors, and depression and anxiety in
children of US born and immigrant parents (Co-I: Max M Aung)
My name is Carlos Cardenas-Iniguez and I am a Postdoctoral Fellow in the Environmental Genomics T32 in the Department of Population and Public Health Sciences at USC. I completed my PhD and MA at The University of Chicago in the Department of Psychology with a specialization in Integrative Neuroscience. In addition to my main research projects focused on structural and social determinants of health and their impact on brain development and behavior, I am deeply invested in initiatives that promote the involvement and advancement of scientists belonging to historically minoritized groups.
I am motivated to pursue this project because I believe it is important to go beyond traditional proxies of built and social environments, such as socioeconomic status (SES; education and income) and race/ethnicity, in order to investigate the specific factors that give rise to disparities in minority mental and physical health. In particular, I am highly interested in exploring these factors in US immigrant communities and fill in gaps in the literature on how this sociocultural context may exacerbate or mitigate stressors in the environment.
I am very grateful to carry out this research with a team of researchers similarly passionate about how research in neuroscience and population health can positively impact communities historically under- or misrepresented in academic discourse.

Nemmi N Cole, PhD
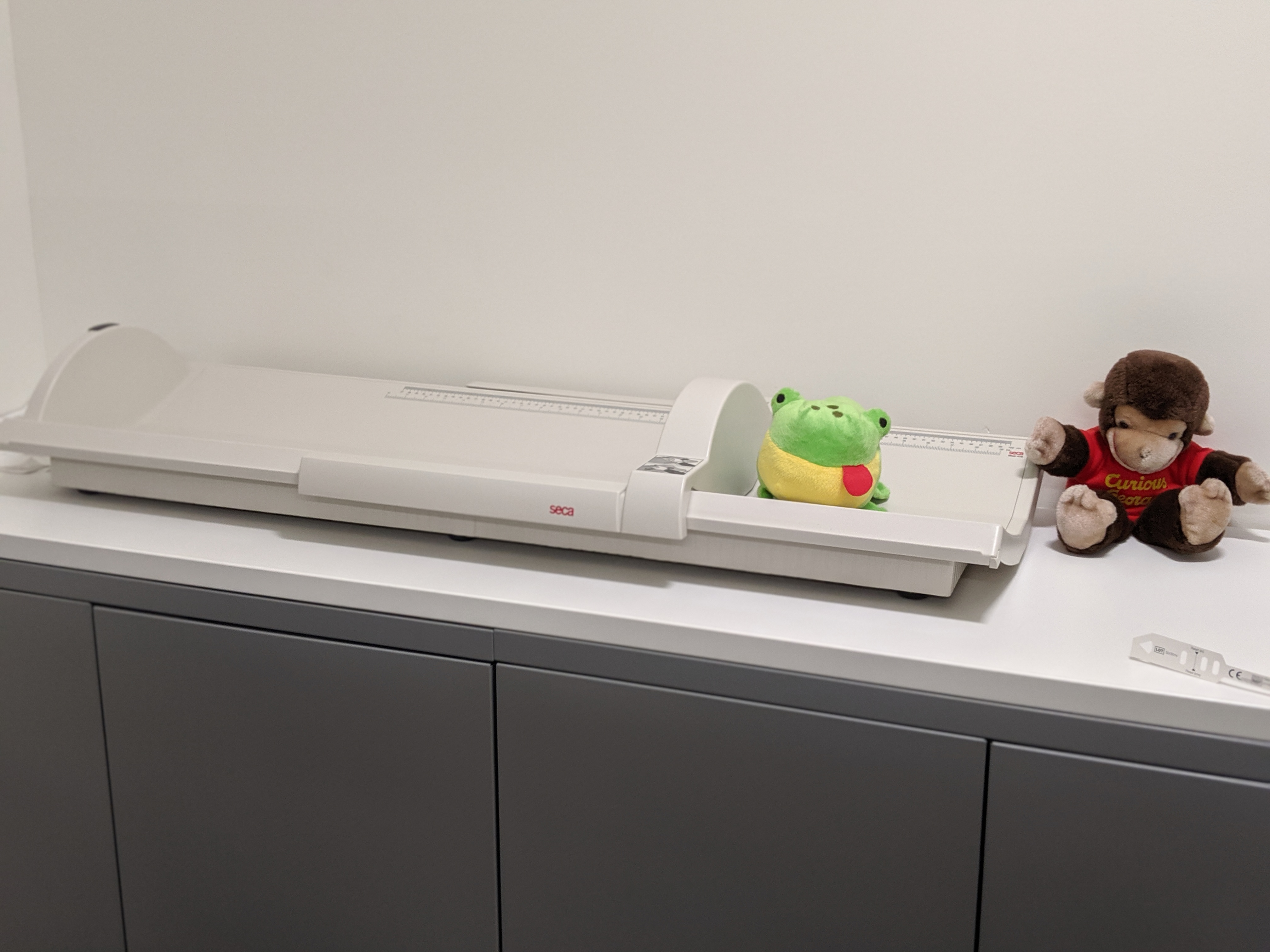
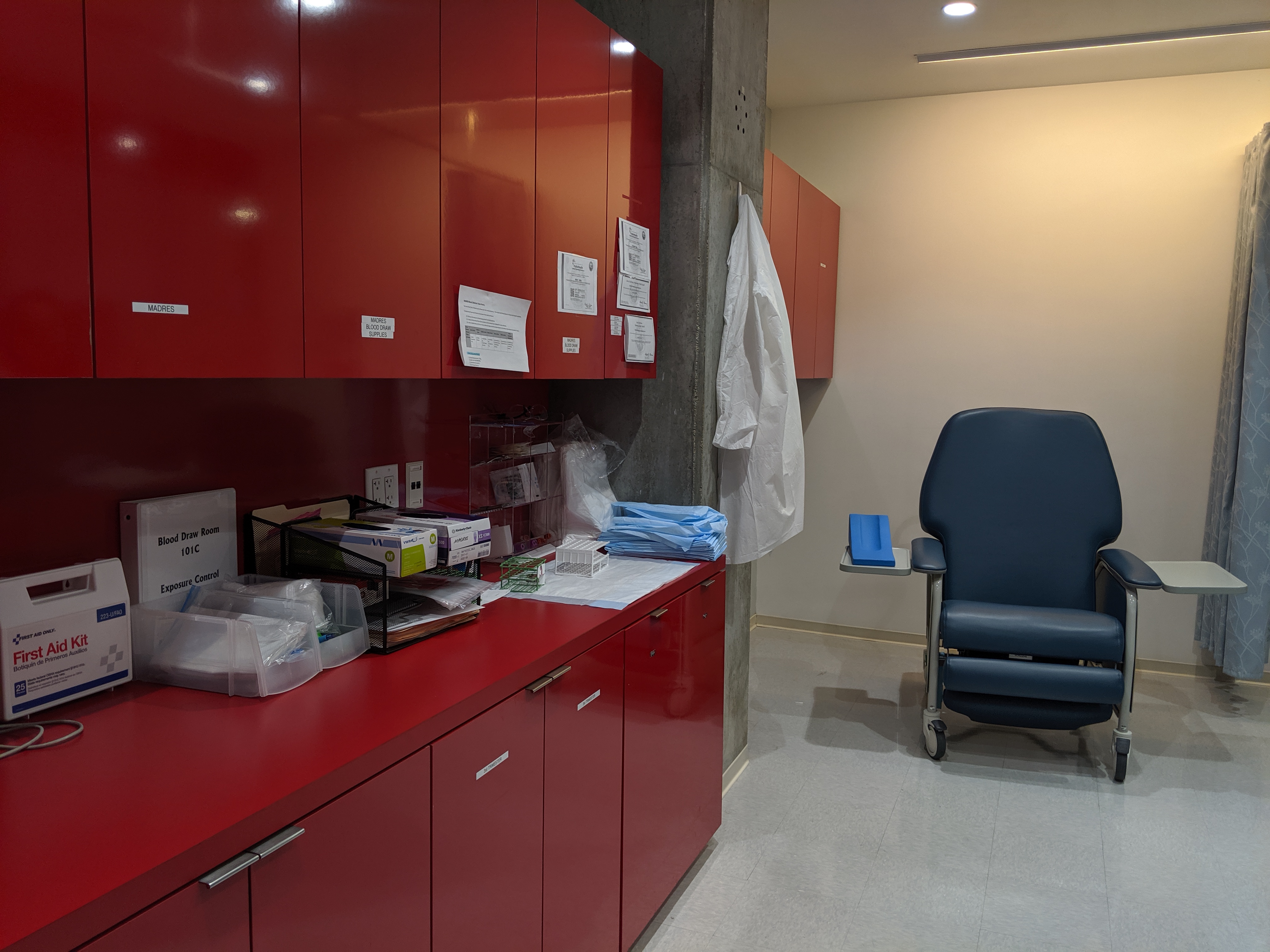
Project Title: Inland Empire Warehouse Development and Children's Respiratory Health Study
I am Nemmi Cole, a Postdoctoral Scholar Research Associate in the Department of Population and Public Health Sciences, Division of Environmental Health at the University of Southern California. I received my Ph.D. in Civil and Environmental Engineering from Florida Agricultural and Mechanical University, FAMU-FSU College of Engineering in 2021.
The key motivation for this project is to address critical gaps in our understanding of the health impacts associated with warehouse developments and warehouse-related externalities on children’s respiratory health outcomes in the Inland Empire region. This study seeks to leverage a community-engaged approach to increase engagement and understanding of exposure risks and advance environmental health literacy.
I am so grateful for the opportunity to pursue this project. I look forward to conducting research that will increase health equity and advance policies to address environmental injustice.
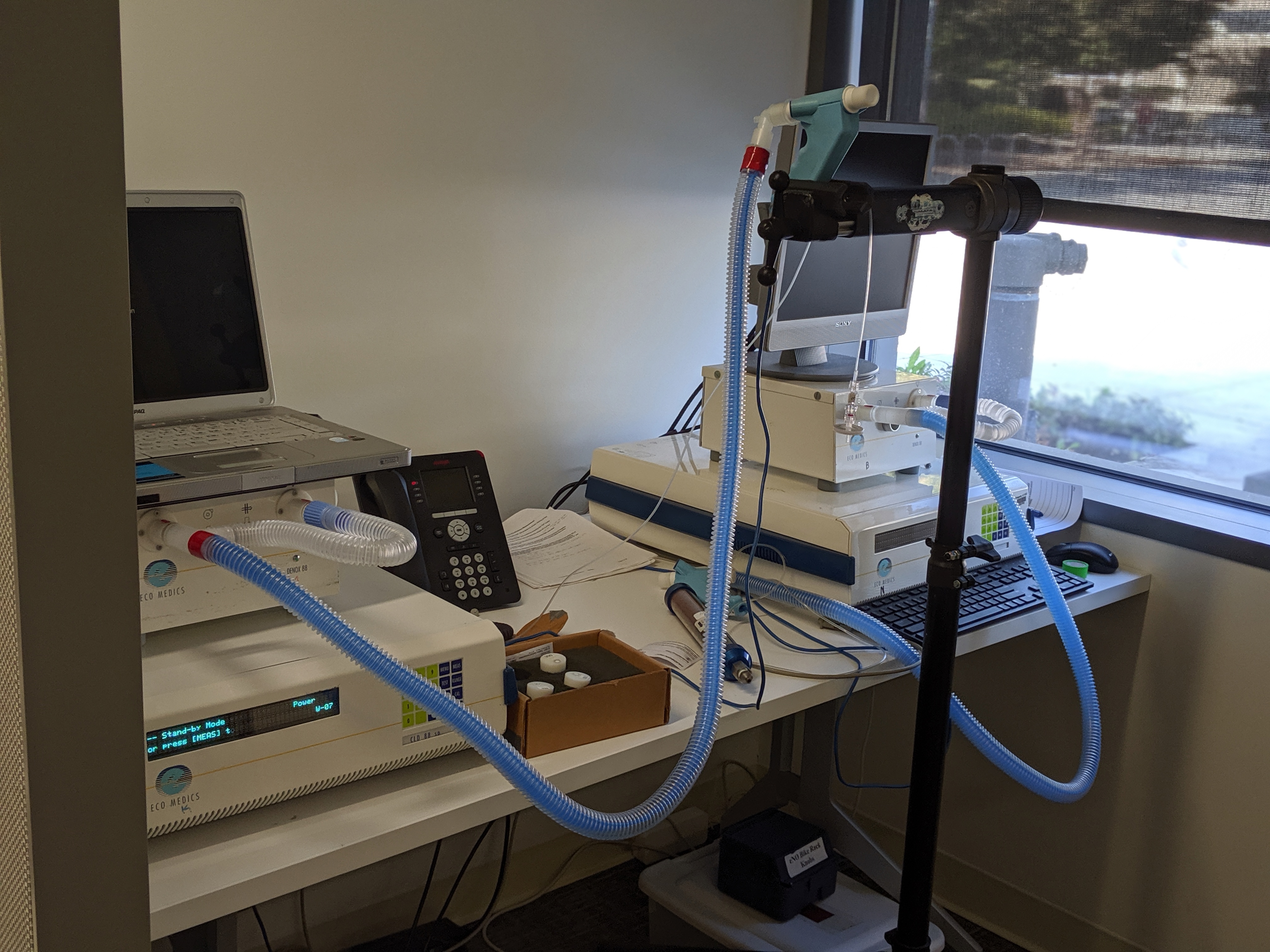
Nan Ji, PhD
Project Title: Neighborhood Socioeconomic Conditions and Disparities in Birth Weight: Investigating Mediation by Prenatal Exposure to Multiple Air Pollutants
My name is Nan Ji and I’m a Postdoctoral Scholar Research Associate at the Department of Population and Public Health Science. I received my doctoral degree at Rutgers University School of Public Health in 2021. My research focuses on the impacts of air pollution on pulmonary and metabolic health, especially in vulnerable populations.
The key motivation for this project is to examine the mediating role of prenatal co-exposure to multiple air pollutants on the association of neighborhood socioeconomic status with birth weight. Evidence of the causal role of air pollution in mediation analyses can guide public health interventions that reduce prenatal exposure to air pollutants, especially among vulnerable populations and to mitigate the adverse aspects of neighborhood conditions, and promote ultimately healthy birth outcomes.

Santiago Morales, PhD
Project Title: Examining the impacts of social context on Latina mothers' and their infants' mental health: An ecological momentary assessment study
Santiago Morales is an Assistant Professor of Psychology in the Developmental and Brain and Cognitive Science areas at the University of Southern California. He received his Ph.D. and M.S. in Developmental Psychology with a specialization in Cognitive and Affective Neuroscience from The Pennsylvania State University. Dr. Morales' research examines early individual differences in the development of emotion and emotion regulation. His research focuses on the impact that these early individual differences have on socioemotional development, especially with regards to the development of internalizing and externalizing psychopathology. Dr. Morales is also interested in examining social and contextual factors that predict these early individual differences. In this project, he is excited to use a new ecological momentary assessment protocol to better understand the effects of sociocultural processes, such as familismo and discrimination, on maternal and infant mental health.