AFFILIATED RESEARCH PROJECTS
In addition to the research projects funded directly by the MADRES Center, multiple other studies utilize the MADRES cohort. These studies investigate additional questions related to the effects of environmental exposures on the health of mothers and their children. Currently, five ongoing research projects are utilizing the MADRES cohort:
- Influence of prenatal psychosocial stressors on maternal and fetal circulating miRNAs: This study investigates the effects of psychosocial and chemical stressors on the pattern of expression of maternal and fetal miRNA, as well as the effects of the expression of miRNA on newborn and early childhood health outcomes. The study makes use of using state-of-the-art technologies to characterize the full repertoire of miRNA.
Learn about the MADRES cohort
Read our article about the MADRES cohort study design, protocol and profile published in BMC Pregnancy and Childbirth.
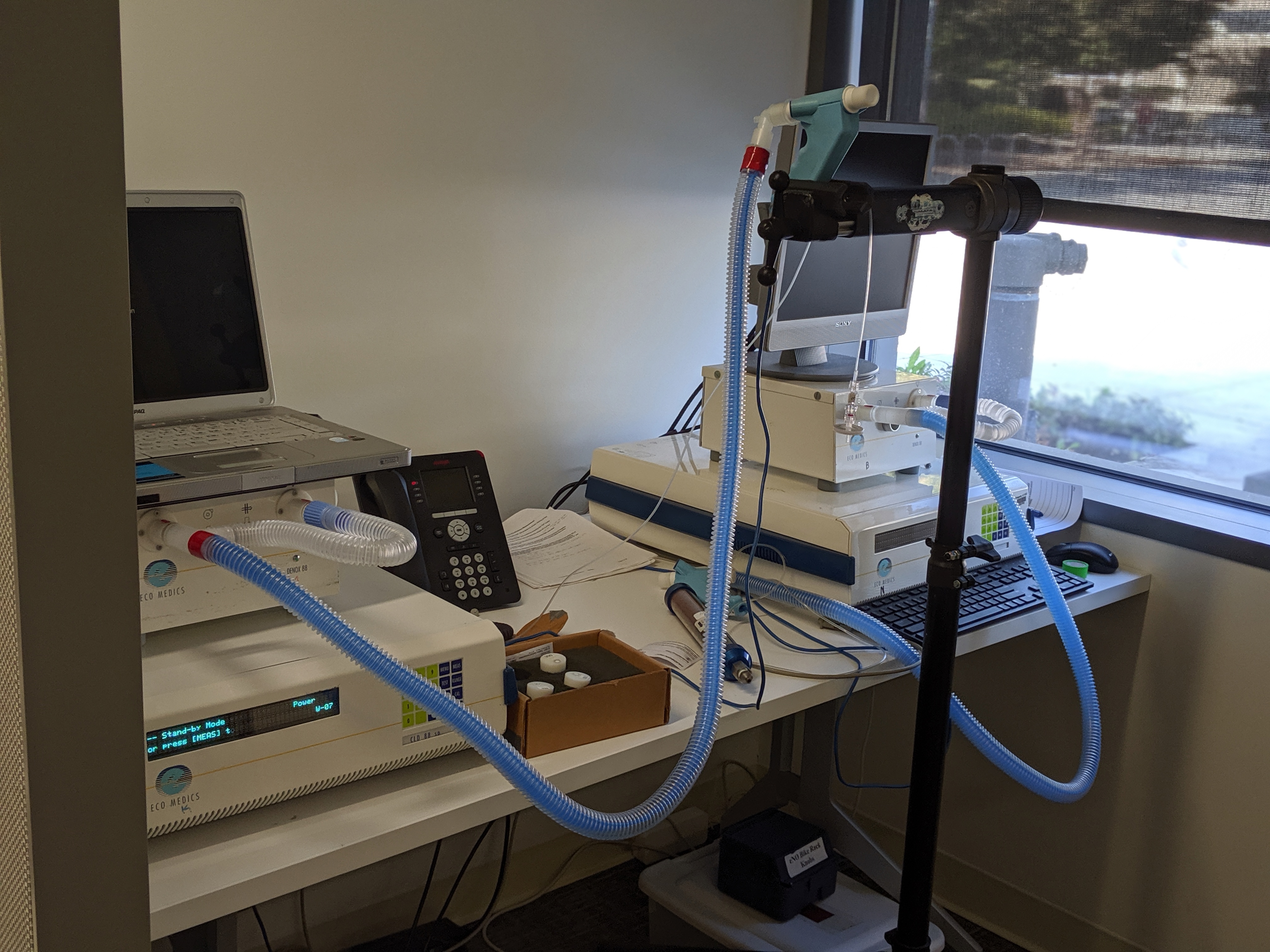
- Lifecourse Approach to Developmental Repercussions of Environmental Agents on MEtabolic and Respiratory health (LA DREAMERs): This project is studying how environmental factors contribute to the origins of childhood and emerging adult respiratory and metabolic health across multiple generations. The study combines 8,931 subjects from the MADRES cohort and the Children’s Health Study (CHS) – two population-based longitudinal cohorts of children that cover the prenatal to early adulthood periods of exposure, focusing on the health effects of ambient and near-roadway air pollution, metals, and novel albumin adducts in a series of three distinct research projects focused on respiratory health, metabolic health, and statistical methods.
- Metabolomic signatures linking air pollution, obesity and diabetes: This study focuses on identifying key metabolic pathways underlying the associations of childhood air pollution exposures with body fat, ectopic fat, and diabetes traits, such as glucose concentrations and insulin resistance, using a metabolomics approach.
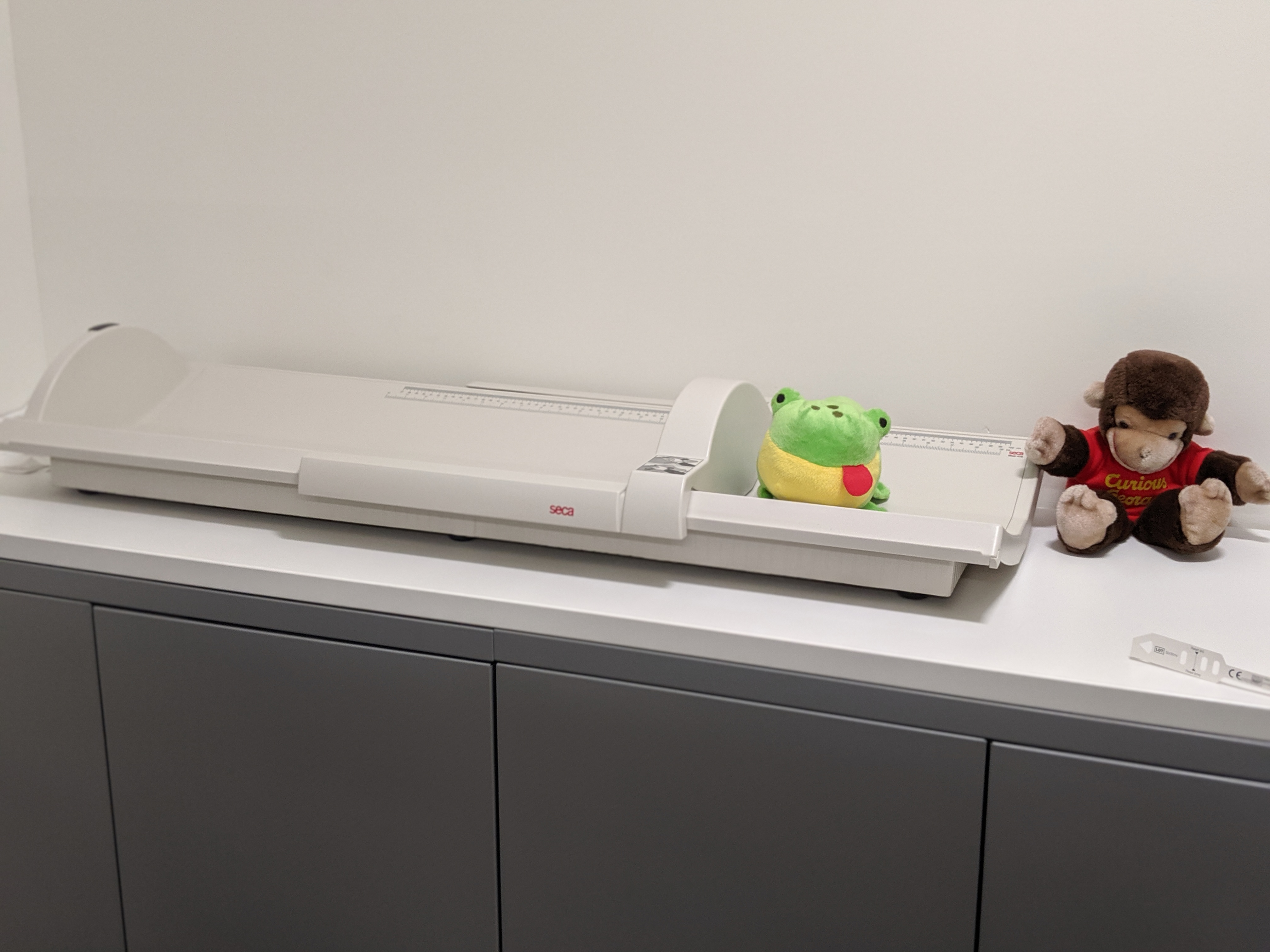
- Prenatal air pollution, fetal development and early childhood obesity risk: This study investigates the role of prenatal environmental exposures to air pollution, and specific constituents of air pollution, using state-of-the-art personal monitoring to reduce exposure measurement error and innovative phenotyping of fetal growth (fetal liver blood flow).
- Prenatal metal mixtures, fetal growth, and the role of microRNAs: This study examines the impact of prenatal metal mixture exposures on fetal growth, as well as the role of altered maternal circulating miRNAs on these relationships, using metals exposure assessment methods, weighted quantile sum regression, and Bayesian kernel machine regression, structural equation models, and RNA-Seq.
To learn more about our cohort research projects, read their abstracts below.
ABSTRACT: The environment experienced by a developing fetus during gestation can have profound impacts on health outcomes throughout life. Infant growth is a significant risk factor for long-term chronic disease, particularly later childhood risk for obesity. A better understanding of the mechanisms through which the environment can program offspring obesity risk may help to improve risk assessment as well as provide opportunities for novel prevention approaches. These efforts may be most needed amongst populations experiencing the greatest health disparities, where adversities in the environment can be psychosocial, physical, and chemical in nature and where these exposures may be acting synergistically to impact health. Epigenetic mechanisms, due to their developmental plasticity but long-term functional role, have been posited as critical mediators of the environment’s impact on children’s health. Non-coding RNA, and particularly, microRNA (miRNA), represent one epigenetic mechanism that functions to control the stability of messenger RNA (mRNA) and the translation of proteins. There is growing evidence that miRNA can act as an inter-cellular signal to modulate various physiologic responses including metabolism and immune response. Due to these roles and their inherent ability to effect large numbers of target genes, miRNA represent fundamental regulators with the potential for wide-ranging consequences. We hypothesize that psychosocial, in addition to chemical stressors, in the maternal environment impact the pattern of expression of maternal and fetal miRNA and that the expression of these miRNA can impact critical newborn and early life health outcomes. We will examine this hypothesis using state-of-the-art technologies to characterize the full repertoire of miRNA in the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) pregnancy cohort, which focuses on low income Hispanic women in Los Angeles county. The MADRES cohort is collecting extensive data on actual objective stressors (negative life events, past trauma, neighborhood disorder) and the psychological response to stress (perceived stress and depression symptoms) along with socio-demographic information to comprehensively understand the extent of psychosocial stress experienced in this population. This proposal will measure miRNA in already collected peripheral blood samples 1st and 3rd trimesters, cord blood samples at birth, and will support the effort to collect placental samples for additional miRNA analysis. The main aims of the proposal will be to 1) examine how maternal psychosocial stress impacts the pattern of expression of miRNA in maternal blood during pregnancy, 2) delineate how maternal circulating miRNA impact newborn health outcomes including birth weight and small-for-gestational birth, and 3) examine the relationship between patterns of expression of miRNA in placental tissue and in cord blood to those in maternal serum. Results of this study will provide evidence for the role that miRNA play in mediating the effects of the prenatal environment on children’s health within a Hispanic population experiencing significant health disparities.
Contact PI: Carrie Breton
Supported by: NIMHD: 5R01MD011698-03
ABSTRACT: Scientific evidence in both humans and animal models suggests that prenatal, early life and potentially transgenerational environmental exposures can result in childhood health deficits and life-long consequences in subsequent generations. In particular, exposures to elevated ambient air pollution, regional and near- roadway pollutants, and heavy metals have been associated with respiratory and/or metabolic health outcomes in childhood. Much less is known about the effects of prenatal exposures on these outcomes, and virtually nothing is known about whether exposures during previous generations can affect respiratory and metabolic outcomes – illustrating critical gaps in scientific knowledge. Studies are just beginning to disentangle the effects of mixtures across the life course using novel biomarkers of exposure, biological mediators and innovative statistical methods. We will address these critical gaps in a new proposal entitled “Life course Approach to Developmental Repercussions of Environmental Agents on MEtabolic and Respiratory health (LA DREAMERs).”The major goal of this proposal is to take a transgenerational life course approach to studying the contribution of the environment to the developmental origins of childhood and emerging adult respiratory and metabolic health. LA DREAMERs will combine 8931 subjects from two population- based longitudinal cohorts of children that cover the prenatal to early adulthood periods of exposure- the Maternal And Developmental Risks from Environmental and Social Stressors (MADRES) and Children’s Health Study (CHS) cohorts. The proposed study addresses the following key questions in the field: 1) Do prenatal and early childhood environmental exposures alter childhood and emergent adult respiratory and metabolic health? If so, are there critical periods of exposure across the lifecourse? 2) What is the role of altered immune functions in the underlying biological mechanisms? 3) Will more precise exposure assessment for ambient air pollutants through application of a national spatiotemporal model or development of biomarkers in neonatal dried blood spots and cord blood allow critical components of the mixture to be identified? 4) Do prenatal environmental exposures induce transgenerational epigenetic alterations that help explain increased risk of disease? 5) Can innovative statistical approaches untangle the effects of exposure mixtures on multiple health outcomes? We will address these important questions by focusing on the health effects of ambient and near-roadway air pollution, metals (As, Pb, Cd, Hg), and novel albumin adducts (e.g. reactive electrophiles such as oxidized polyaromatic hydrocarbons and quinones) in a series of three distinct research projects focused on respiratory health (ECHO Focus area #1), metabolic health (ECHO Focus area #2) and statistical methods. By combining MADRES and CHS, we are uniquely positioned to answer environmental health questions pertaining to respiratory and metabolic health using a transgenerational life course approach, spanning from pregnancy through 22 years of age and across generations.
Contact PI: Frank Gilliland
Supported by: NIH OD: 5R01MD011698-03
ABSTRACT: The emergent evidence indicates that exposures to regional air pollutants (AP) and near-roadway air pollutants (NRAP) are associated with the development of obesity and type 2 diabetes. Previous studies suggest that prenatal and early life exposures to AP may play critical roles in the etiology of childhood obesity. However, the mechanism linking AP exposures and obesity and diabetes is unknown. Studies investigating the pathogenesis of the AP-related obesity and diabetes etiology are urgently needed. Metabolomics technology provides epidemiologists and clinicians an unprecedented opportunity to examine the metabolic pathways linking exposures and disease traits. In this proposal, the candidate proposes to identify key metabolic pathways underlying the associations of childhood AP exposures with body fat, ectopic fat and diabetes traits such as glucose concentrations and insulin resistance via the metabolomics approach. Studies involved in the K99 and R00 phases encompass two important developmental periods (neonatal and adolescence). Therefore, this work may elucidate the critical periods of AP exposures that accelerate and/or alter the course of disease, and will potentially inform us with novel molecular targets for early intervention and prevention of obesity and diabetes. In the K99 mentored phase, the candidate will pair new measurement of targeted metabolomics of amino acids and fatty acids with existing AP exposure data and obesity and diabetes phenotypes in an ongoing substudy of the prospective Children’s Health Study (CHS), which is examining the metabolic health impacts of AP exposure in Southern California. Targeted metabolomics will be used to identify pathway(s) of amino acid and fatty acid metabolism that are associated with cumulative exposures to regional AP and NRAP from prenatal to adolescence, as well as metabolic disease traits in 200 CHS adolescents. Additionally, specific metabolites such as acylcarnitines and fatty acids will be analyzed to examine the hypothesized mechanism linking air pollution and obesity and metabolic disorders, such as inflammatory activation and leptin resistance. The proposed training objectives during the K99 phase, which includes personal mentorship, didactic courses and research seminars, meetings, and workshops, are designed to enhance the candidate’s knowledge and skills in four essential areas including 1) exposure assessment and environmental epidemiology, 2) metabolomics, 3) statistical modeling specific to metabolomics data and mediation analysis, and 4) career development. The accomplishment of the proposed training in the K99 phase will ensure the candidate to successfully conduct the K99/R00 research projects and to be well-equipped for future transition into an independent environmental health scientist. In the R00 phase, the candidate will apply the training and skills developed during the K99 phase on a prospective birth cohort study, the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) Study. The candidate will use the non-targeted metabolomics to discover novel metabolomic signatures related with prenatal AP exposures and neonatal and infant adiposity among 250 cord blood samples from the MADRES. Subsequently, targeted metabolomics will be analyzed in the cord blood samples from an independent group of 250 newborns from the MADRES to replicate previously identified metabolomic signatures. Both K99/R00 projects will fill critical gaps in our understanding of the metabolic pathways linking prenatal and chronic AP exposures and the development of childhood obesity and metabolic disorders. With the proposed projects and essential training obtained during the K99 phase, the candidate will be positioned to initiate her independent academic career and to carry out novel research to decipher the disease etiology related with environmental exposures, and to discover new cellular and molecular targets for early intervention and prevention of obesity and diabetes.
Contact PI: Zhanghua Chen
Supported by: NIEHS: 4R00ES027870-03
ABSTRACT: A growing body of evidence suggests that prenatal and early-life exposures to environmental stressors play a role in the etiology of multiple childhood health outcomes including childhood obesity and metabolic dysfunction. One pervasive exposure of concern is particulate air pollution. Prenatal exposure to air pollution has been associated with adverse fetal growth outcomes, including decreased biparietal diameter, head and abdominal circumference, femur length, and low birth weight. At the same time, prenatal air pollution has also been associated with increased risk for childhood obesity. One explanation for this apparent paradox is a fetal programming hypothesis, which holds that a maladaptive intrauterine environment leads to an adaptive response that alters the fetal metabolic and hormonal milieu designed for intrauterine survival. Thus, growth restriction in utero is associated with greater catch-up growth in infancy and obesity risk later in life. A more sophisticated metric of fetal development—the Doppler ultrasound assessment of umbilical venous perfusion of the fetal liver—also influences fetal growth by prioritizing nutrient allocation for prenatal fat deposition when essential nutrients are plentiful. Moreover, the adipokines leptin and adiponectin play key roles in fetal- maternal metabolism. We hypothesize that air pollution decreases fetal growth and negatively alters fetal liver blood flow which in turn increases the risk of catch-up growth and obesity in later childhood. We further hypothesize that adiponectin and leptin may mediate these observed effects. We will investigate these hypotheses in a subset of 500 participants in the longitudinal pregnancy cohort of low income, predominantly Hispanic, pregnant women known as the Maternal And Developmental Risks from Environmental and Social Stressors (MADRES) Cohort. The specific aims include investigating the effects of personal prenatal air pollution (NO2, BC, BrC, PM2.5 mass, its components and sources) exposure on 1) ultrasound-derived fetal growth measures and 2) childhood adiposity and early childhood growth trajectories from 0 – 2 years, 3) whether associations are modified by maternal BMI, GDM, and infant sex, and 4) whether protein levels of leptin and adiponectin in maternal serum, placenta, and cord blood mediate associations between air pollutant exposures and infant growth and adiposity. This proposal addresses a critical gap in our current understanding of the etiology of childhood obesity risk by investigating the specific role of prenatal environmental exposures to air pollution, and specific constituents of air pollution, using state-of-the-art personal monitoring to reduce exposure measurement error and innovative phenotyping of fetal growth (fetal liver blood flow).
Contact PI: Carrie Breton
Supported by: NIEHS: 5R01ES027409-02
ABSTRACT: Reduced fetal growth has been implicated in a broad range of adverse health outcomes. Growing evidence suggests that toxic metal exposures adversely affect fetal growth, indicated by reduced fetal ultrasound measurements and lower birth weight. Although most individuals are exposed simultaneously to multiple metals, which may act additively or synergistically to reduce fetal growth, the majority of studies have focused on the toxicity of individual metals. While the mechanisms underlying metal-induced reductions in fetal growth are incompletely understood, there is evidence that epigenetic dysregulation, including altered microRNA (miRNA) expression, contributes to these effects. In addition to epigenetically regulating gene expression, maternal circulating miRNAs play important roles in maternal-placental-fetal crosstalk. However, the potential role of maternal circulating miRNAs in mediating metal mixture effects on fetal growth is unknown. The goal of the proposed project is to examine the impact of prenatal metal mixture exposures on fetal growth and to determine whether altered maternal circulating miRNAs mediate these relationships. During the mentored K99 phase of this award, Dr. Howe will leverage existing data and biospecimens from 500 mother-newborn pairs in the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) study, a low- income predominately Hispanic pregnancy cohort based in Los Angeles, to investigate potential additive and synergistic relationships between prenatal exposure to 15 metals and in utero growth and birth weight. To accomplish this, she will expand metals exposure assessment in the MADRES pregnancy cohort and train in methods for analyzing complex environmental mixtures, including weighted quantile sum regression and Bayesian kernel machine regression. During the R00 phase, Dr. Howe will determine whether maternal circulating miRNAs mediate metal mixture-fetal growth relationships, using structural equation models, and will examine potential downstream effects by profiling mRNA expression levels within the maternal-placental-fetal axis, using RNA-Seq, in a subset (N = 50) of mother-newborn pairs. Results from the proposed studies may be used to improve the efficacy of public health interventions aimed at preventing metal-induced reductions in fetal growth. Furthermore, they will increase knowledge of a potential underlying mechanism (altered maternal circulating miRNAs) and may lead to the identification of early and relatively non-invasive biomarkers of metal mixture exposures and reduced fetal growth. Dr. Howe has assembled a mentoring team, spanning the University of Southern California, Boston University, and Emory University, with expertise in metals toxicity, environmental mixtures modeling, epigenetic epidemiology, and perinatology. This team will provide ongoing feedback and on-site training opportunities to complement coursework, workshops, and seminars, which will support Dr. Howe’s transition to become an independent investigator with a research program that focuses on the effects of early life metal mixture exposures on the epigenome and fetal growth.
Contact PI: Caitlin Howe
Supported by: NIEHS: 1K99ES030400-01